Why Is Your Patient's Baby Breech or Transverse?
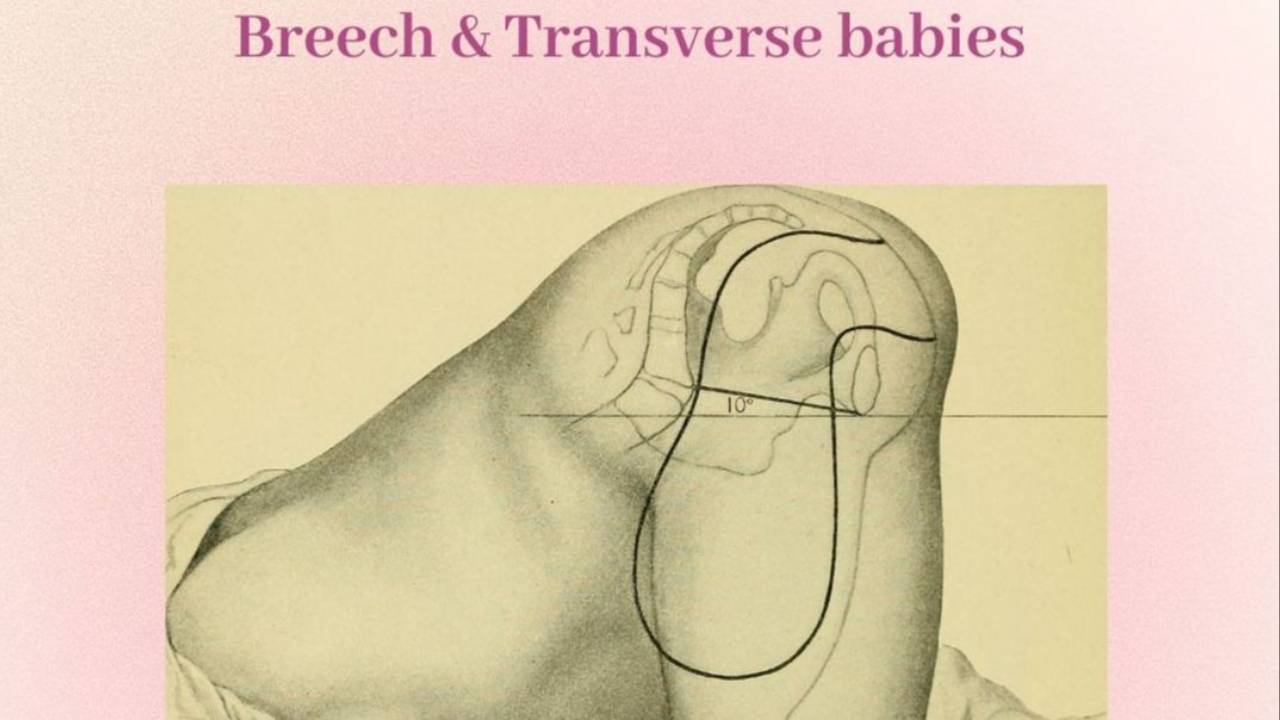
A breech presentation refers to a baby positioned in the uterus with their buttocks or feet (or one foot) down, rather than the typical head-down position expected for birth. This is relatively common earlier in pregnancy, but most babies turn head-down by the third trimester. If the baby remains breech closer to term, it may influence how delivery is planned.
There are a few different types of fetal positions that can affect delivery:
- Breech: Baby’s bottom or feet are closest to the cervix. This can be further classified into frank breech (bottom down, legs up), complete breech (bottom down, legs crossed), or footling breech (one or both feet first).
- Transverse lie: Baby is lying sideways across the uterus, rather than vertically. This position makes vaginal delivery impossible unless the baby turns.
- Oblique lie: Baby is positioned at an angle, neither fully vertical nor horizontal. This is often a transitional position that may resolve on its own.
Understanding these positions—and what might contribute to them—can help you treat your patient or client more confidently. In the rest of this article, we’ll cover the common reasons a baby might be breech, ways to support optimal positioning, and how conservative therapies like those taught at the Integrative Somatic Healing Institute can help.

When is breech position diagnosed?
A breech presentation is usually diagnosed as early as the 20-week appointment, or at a further appointment around 28–30 weeks during a routine prenatal visit. If breech is suspected, palpation or an ultrasound may be done, typically between 32–36 weeks, to confirm the baby’s position and check for other factors.
Is Breech delivery safe?
In the past, OBs and midwives were trained to assist with breech deliveries. However, in recent years, many hospitals have moved away from allowing breech vaginal births due to safety concerns and liability issues. That said, some providers with additional training may still offer vaginal breech deliveries under specific conditions, approving them on a case-by-case basis. Despite this, a significant number of OBs and midwives continue to recommend elective C-sections when the baby is breech.
6 Common Reasons for Fetal Malpositioning Explained
While there’s no single proven cause for why a baby may be breech, several factors can contribute:
1. Myofascial Tissue Tension Around the Uterus
Soft tissue tension around the uterus, particularly in the fascia, ligaments, and surrounding muscles, can impact the alignment of the pelvic inlet and midpelvis. The baby’s head (the largest part) needs adequate space to settle into the pelvis. If that space is restricted, the baby’s buttocks or feet (being smaller) may settle there instead, contributing to a breech position.
The shape and structure of the pelvis and uterus can significantly influence your baby’s position. For example, a bicornuate (heart-shaped) uterus or the presence of fibroids may limit space or create uneven contours that make it harder for the baby to rotate into a head-down position.
Likewise, a tight or asymmetrical pelvis—whether due to genetics, previous injury, or muscle tension—can restrict movement and affect how the baby settles.
Additionally, a history of pelvic floor muscle dysfunction—such as pelvic pain, vaginismus, constipation, or chronic tension—has been clinically associated with a higher rate of breech babies.
Certain activity patterns may also play a role. High-intensity workouts which create a lot of hip & pelvic muscle tone such as running, CrossFit, spinning, or heavy weight lifting (especially more than 3–4 times per week) can contribute to elevated pelvic floor tone. Some Pilates practices, particularly those that emphasize repetitive tailbone tucking, may reduce tailbone flexibility and mobility, which correlates with transverse, oblique, and breech positions.
Lastly, wearing restrictive clothing or tight belly bands for extended periods may also affect fetal positioning. Overuse of external support can hold the abdominal muscles up too much, limiting the natural drop of the uterus and making it harder for baby to engage in the pelvis—potentially affecting positioning and delaying labor onset.
Click the video below for a patient-friendly explanation :
How can pelvic floor therapy help?
At the Integrative Somatic Healing Institute (ISHI), we teach pelvic health therapists gentle manual therapy techniques that can create more space and mobility in the pelvis—key factors in supporting optimal conditions for babies to turn into a head-down position.
Our approach includes both external and internal techniques designed to improve the flexibility and balance of the pelvis, addressing restrictions in muscles, ligaments, and joints that may be influencing the baby’s position.
We’re proud to teach a dedicated breech protocol, a specialized treatment approach developed specifically for expecting mothers with breech babies. This protocol is unique to ISHI and is performed exclusively by our trained providers. It incorporates hands-on techniques that support the body’s natural ability to align and release tension, while also creating a calm, supportive space for emotional processing that may be affecting your client's experience of pregnancy and baby positioning.
2. Too Much or Too Little Amniotic Fluid
Amniotic fluid acts like a cushion and allows a baby to move and rotate throughout pregnancy. When there’s too much fluid (a condition called polyhydramnios), the baby may move excessively, making it harder for them to stay in one position—especially head-down. On the flip side, too little fluid (oligohydramnios) can reduce the space available and limit your baby's ability to turn.
Your patient should seek advice from their medical provider regarding possible interventions to manage a healthy level of amniotic fluid, We discuss some wellness based strategies in our Integrative Pelvic Care for Pregnancy course - more details here.
3. Placenta Placement
Where the placenta attaches inside the uterus can also influence the baby’s position. If the placenta is lying low and covering part or all of the cervix (known as placenta previa), or if it’s anterior (on the front wall of the uterus), it might physically block or discourage the baby from turning head-down. This can change how your provider approaches your patient's care and may be something they monitor closely in the third trimester.
4. Multiple Pregnancies
In twin pregnancies, the likelihood of one or both babies being breech is notably higher. Approximately 30-40% of twin pregnancies result in one or both babies being in a breech position at some point before birth. In many cases, the first twin is more likely to be in a head-down position, while the second twin is at higher risk for being breech.
5. Prematurity
Earlier in pregnancy it’s very common for babies to be in a variety of positions, including breech. In fact, studies show that about 25–30% of babies are breech at 28 weeks, but most will naturally turn head-down with only 7% of babies being breech at 32 weeks.
By 37 weeks, only about 3–4% of full-term babies remain in the breech position. However, if a baby is born early (before full term), the chance of remaining breech increases simply because there hasn’t been enough time for the baby to rotate into the head-down position.
If your patient's baby is in a breech, transverse, or oblique alignment at 32 weeks, it is very important to provide them with movement and manual therapy interventions based on our Breech Protocol, to give the baby the best chance of being in a head-down or vertex alignment for birth.
6. Emotional or Energetic Blockage
While structural factors often play a role in a breech presentation, they’re not the whole story. Emotional and energetic influences—such as stress, fear around birth or motherhood, or even a history of trauma—can also impact your baby’s position. That’s why it’s so important to care for your emotional well-being during pregnancy, not just your physical health.
At the Integrative Somatic Healing Institute, we equip clinicians with strategies to gently guide expecting mothers into increased emotional awareness and supported release of their birth-related fears. By creating space to explore what might be showing up—whether consciously or beneath the surface—we aim to support both mother and baby in finding balance. When deeper layers emerge that may need additional care, we help ensure you’re supported in a way that honors your full experience.
If you’re patient's baby is breech, know that you have treatment options—and you have us to guide you along.
While some situations may ultimately require medical intervention, many expecting mothers benefit from starting with conservative mind-body therapy that support optimal pelvic alignment, mobility, and nervous system regulation.
At Integrative Somatic Healing Institute, we help you master gentle, non-invasive techniques that encourage your patients' baby to turn naturally while also supporting their overall well-being.
If you’re curious about how we can support you, reach out at [email protected] or learn more about our breech support offerings.

